mRNA vaccine cold chain challenges threaten widespread access across African healthcare systems
Thermal instability of revolutionary technology demands innovative solutions to overcome distribution barriers in resource-limited settings.
May 29, 2025

Among the COVID-19 vaccines distributed globally, mRNA-based vaccines demonstrated the highest efficacy. These mRNA vaccines showcase their ability to develop and manufacturing capabilities, which make them revolutionary tools compared to traditional vaccine types, particularly when pandemics occur.
According to the World Health Organization, more than 40 different mRNA vaccines that target COVID-19 are under clinical trials. Similarly, beyond the scope of just COVID-19, many other mRNA-based candidates for prevention and control of infectious diseases like influenza, cancer, and other genetic disorders are also in clinical trials.
However, despite their advantages in efficacy and speed of development, mRNA vaccines come with major limitations which chief among them being thermal instability and the need for ultra-cold storage conditions. Unlike conventional vaccines that can typically withstand standard refrigeration, data provided to the European Medicines Agency reveal that storing Moderna’s vaccine at 2-8°C shortens its shelf life from six months to only 30 days, while Pfizer-BioNTech’s is reduced to just five days.
According to the World Health Organization, more than 40 different mRNA vaccines that target COVID-19 are under clinical trials.
These limitations are particularly problematic in regions like Africa, where cold chain infrastructure is limited. The strict temperature conditions needed for major mRNA COVID-19 vaccines are shown in Figure 1.
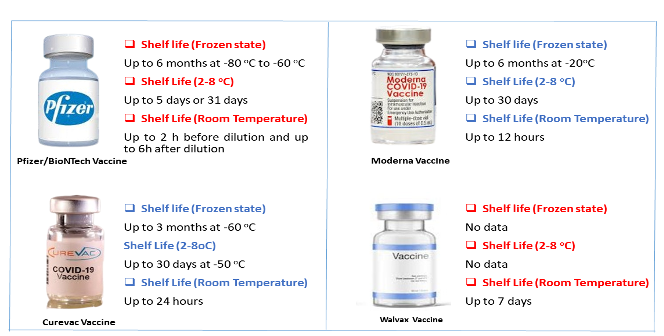
Figure 1: mRNA COVID-19 vaccines temperature control requirements. Data from Uddin and Roni (2021).
Overcoming cold chain limitations for mRNA Vaccines in Africa
According to the Agency for International Development (USA), millions of vaccines are wasted globally, with broken cold chain systems being one of the leading causes in Sub-Saharan Africa. Maintaining the necessary environment for mRNA vaccines is particularly difficult in underdeveloped nations where frequent power outages occur, ultra-cold facilities are scarce, and minimal funding for advanced infrastructure.
The consequences of failing to maintain the cold chain requirement become profound as public health efforts are placed at risk when failed attempts to maintain the thermo-stability of mRNA vaccine led to loss of potency and ineffectiveness upon administration during immunisation. This scenario is a critical issue, especially as Africa looks to expand its vaccination programmes, not just for COVID-19 but also for other diseases such as malaria and HIV, where mRNA-based vaccines may play a future role.
Maintaining the necessary environment for mRNA vaccines is particularly difficult in underdeveloped nations
According to 2025 research by Talbot et al. the major bottleneck in the deployment of mRNA vaccines across Africa is the disparity between urban and rural cold chain capacity. In many settings, vaccines must travel long distances from central hubs to health centres, often under unreliable temperature control.
A study in Cameroon documented that 96% of vaccine supplies faced temperature levels higher than 8°C for extended durations exceeding ten hours at their distribution points and within facilities.
The vulnerability of cold chain systems throughout the region constitutes a wide-reaching concern since vaccines face heightened risks of deterioration while being transported. This cold chain limitation became more evident as several African countries were unable to store or distribute mRNA vaccines during the peak of the COVID-19 pandemic period because they lacked needed ultra-cold freezers. While global assistance like the UNICEF’s delivery of 800 ultra-cold chain freezers to nearly 70 countries in 2021 helped but significant gaps remain. Even when cold chain infrastructure is installed, problems arising from power outages that can extend beyond scheduled durations and insufficient local technical capacity continue to pose ongoing threats to cold chain reliability across the continent.
The vulnerability of cold chain systems throughout the region constitutes a wide-reaching concern since vaccines face heightened risks of deterioration while being transported.
To address these hurdles, solutions like solar-powered refrigerators have been promoted, especially in areas with fewer than eight hours of daily electricity. GAVI recommends these for low-resource settings, and while they offer hope, their effectiveness is constrained by high cost, dependence on stable energy inputs, and maintenance demands. More sustainable progress requires a shift from simply reinforcing cold chains to addressing the root of the problem of mRNA vaccine thermostability. Instead of relying solely on refrigeration, investment must go into developing heat-stable mRNA vaccines that can withstand higher temperatures without losing potency. While partnerships like the Africa CDC and Mastercard Foundation’s Saving Lives and Livelihoods initiative are strengthening distribution capacity, long-term vaccine access will depend on scientific innovation that removes or reduces reliance on fragile temperature-dependent logistics.
Implications for the future
The evolving of mRNA vaccine technology and its corresponding application is expected to extend beyond COVID-19, as it offers promising avenues for other diseases like HIV, malaria, and cancer. Given this expected growth, research aimed at stabilising mRNA vaccines against heat degradation must be facilitated to accommodate this anticipated long-term presence of mRNA vaccines in healthcare systems. Vaccines that remain stable at higher temperatures could lessen the reliance on ultra-cold storage and significantly improve vaccine availability.
Conclusion
The long-term effectiveness of mRNA vaccines in Africa depends on both advancing scientific research and strengthening logistical capabilities. Research priority should be placed on understanding how mRNA deteriorates and the ways to boost its resilience. The true impact of this transformative vaccine technology will only be achieved in developing countries when it is both effective and reachable, irrespective of location or existing infrastructure.
References available on request.
Get exclusive in-person access to the latest laboratory innovation and trends in Africa by registering at WHX Lagos.


